Spinal Cord Injury involves temporary or permanent damage to the spinal cord, part of the central nervous system that runs down the middle of the spinal column. The spinal cord carries information from the periphery to the brain and back, and damage to it can result in loss of sensation and both voluntary and involuntary function of large parts of the body.
How can the spinal cord be injured?
Damage to the spinal cord can occur in multiple ways, but primarily it involves trauma. Road traffic accidents and falls are the most common. This can involve a slipped disc pressing on the spinal cord, or a fractured vertebra either damaging or pushing on the cord. Other causes include infection, lack of blood flow (ischaemia) and tumours. Just over half of all spinal cord injury occurs in the cervical spine, the region in the neck.
Clinical Features/ Symptoms
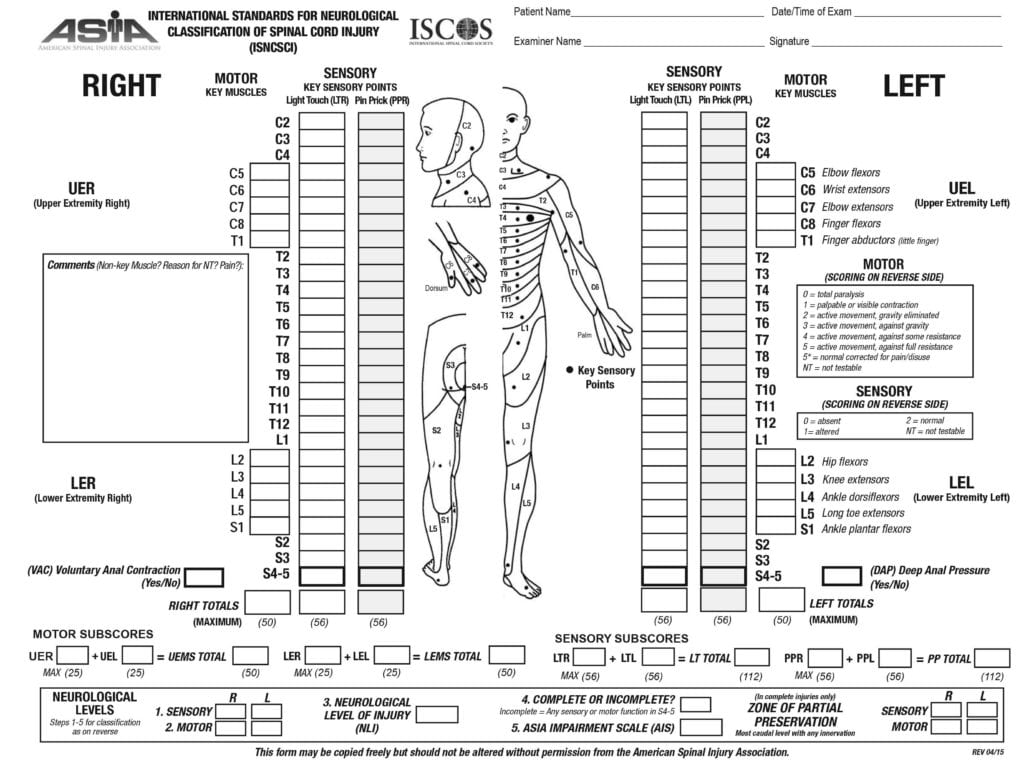
Spinal cord injury is usually graded using the American Spinal Injury Association Impairment Scale.
Whilst this helps us in terms of understanding the total impact of the injury on function, symptoms can vary depending on the location of damage.
Some of the more common types are considered incomplete injuries because not all of the spinal cord is compromised.
Though rather commonly damaged, we aren’t going to discuss the cauda equina – the horsetail like bundle of nerves branching off below the spinal cord here for streamlining purposes.
Lastly, it should be noted that Complete Spinal Cord Injury is the most drastic of all injuries since by definition, neither your motor nerves (responsible for moving) or sensory nerves (responsible for feeling) can communicate with the brain at all. This usually arises from a very significant traumatic event such as a severe accident or penetrating injury such as a gunshot, and is associated with the worst ASIA scores.

Investigations/Diagnosis:
A full neurological examination is vital to understand exactly where function and sensation has been lost. Since your body’s skin territories and muscle groups correspond to particular nerves that come from the spine, examination can also help identify the spinal level where the injury has occurred, especially if imaging is not immediately available.
In the end though, imaging is essential to assess the damage. A CT scan or MRI helps to collate a series of images of the region, vital for determining the exact sites of injury and the extent of any blood vessel damage, fractures, bruising or loss of cerebrospinal fluid (CSF) from the spinal canal. If we can identify where and what is causing someone’s symptoms, then we can plan the best course of action for treatment.
Management/ Treatment
Managing a spinal cord injury depends on its mechanism and location. If it has been caused by trauma for example, immobilisation of the spine as soon as possible is vital in most cases, along with either conservative or surgical correction of any additional spinal injuries. Likewise, if it’s in a certain location, the actual surgical procedures used to fix the damage may differ.
Surgical correction typically involves removing the vertebral bone above the injury site, as well as any blood or any fragments of disc, all to relieve the pressure. The commonest of such procedures is known as a decompressive laminectomy (link to Peter’s article), but screws and rods may be put in to stabilise the spine if required.
Any compressive damage caused by tumours may involve an operation to remove them.
Post Treatment – Rehabilitation
Spinal rehab is complex and different for each patient. It is essential that you and the team looking after you have clear goals set between you to help achieve the best outcomes as you move forward after your surgery.
Rehabilitation is a multi-disciplinary approach.
Doctors will often discharge a patient to a team of specialists with a supply of pain relief focused on relieving nerve pain and laxatives to help you open your bowels. Your recovery would be treated with both its physical and psychological components taken into account.
Physically, physiotherapists work on mobility. This will involve walking aids and perhaps even low-level electrical stimulation to help your muscles re-adjust after the injury.
Occupational therapy meanwhile works on your upper limbs and how well you can do your normal activities, helping to create living quarters where you are well supported and at low risk of any further injury.
Lastly, specialist rehab nurses will help move you to stop you developing pressure sores, which can affect up to 25% of chronic spinal cord injury patients. If loss of bladder and bowel control is present, they will while also monitor their functions so you don’t have accidents and infection can be minimised.
Psychologically, psychologists can help you with any emotional or behavioural concerns while speech and language therapy can aid your swallowing and communication should you have any difficulty.
Finally, case and social workers act as a bridge between each specialist group to streamline your care.
Final notes
Spinal cord injury is a beast with many faces, and unfortunately positive outcomes cannot be guaranteed, even after surgery. It should be noted however that for incomplete injuries treated swiftly, with appropriate and high quality rehabilitation, people can have major improvements up to 18 months. For those with more severe injuries, outcomes can be more bleak, but once again, with appropriate medication and rehabilitation, there is no reason that a patient can’t still salvage a good quality of life regardless.
Brief Summary
- The Spinal cord can be damaged in 6 ways (5 incomplete, 1 complete)
- That main way this happens tends to be traumatic injury from a fall or vehicle accident
- Large variation in severity of injury, depending on mechanism and location
- Imaging and neurological exam are important for diagnosis
- Rehabilitation is complex and requires multi-disciplinary goal setting for the patient to achieve their best outcomes.

Euan Ramsay
Brainbook Student AmbassadorEuan is a medical student with a keen interest in neurosurgery. He regularly contributes to the Brainbook platform and writes science communication articles.

Merlin Strangeway
Medical IllustratorMerlin is an award-winning Medical Illustrator, Writer, Educator and Director of ‘Drawn to Medicine’ and founder of the online illustration school ‘Inktuition’. She strives to visualise information in a way that makes it inclusive, engaging and just for both clinicians, patients and the general public..

Leave a Reply