Phantom meaning false, or not present, phantom limb pain refers to the fascinating phenomenon wherein the mind believes a body part is still attached, and experiences neuropathic pain in that place. Neuropathic meaning due to a lesion or disease of the somatosensory system.
This blog post will delve into what we currently know about the cause, clinical features and treatment of the phenomenon.
Causes
This occurs following an amputation and is positively correlated with the presence of preamputation pain or the amputation site.
For a long time, phantom limb pain was thought to be solely a psychiatric illness. But as science advances, more psychiatric conditions are recategorised as neurological phenomena.
There are three current theories:
- Psychogenic mechanism –
This is where social factors or underlying psychiatric conditions are used to explain the pain.
- Peripheral mechanism –
This looks to stumps and neuromas at the amputation site. The stump left has disrupted nerve signalling, which may lead to neuron hyperactivity causing the pain. A neuroma is a nerve tumour, and this also causes disrupted nerve signalling, causing pain from nerve hyperactivity.
- Central neural mechanisms –
The term neuropathic pain falls into this explanation, and there are 3 forms of central neural mechanisms overall:
The first is where the peripheral or distant ends of the spinal cord sprout new axons into surrounding receptive fields, coupled with increased activity in the neurones. This process is called sensitisation.
Whilst sensitisation is occurring, there is increased activity in NMDA receptors in the spinal cord. This activity leads to up-regulation of these receptors, causing an imbalance in the normal neural firing.
So now we have receptor fields that are more sensitive, and increased neural firing. These collectively lead to overstimulation and hence phantom limb pain.
The second central neural mechanism is due to brain changes. The sensory and motor homunculi in the brain represent a sensory and motor map of the body respectively. Following amputation, these maps are taken over by remaining body areas. This explains why stimulation of the neurones within the stump or surrounding amputation area cause phantom limb pain – the homunculus in the brain for the amputated leg is stimulated.
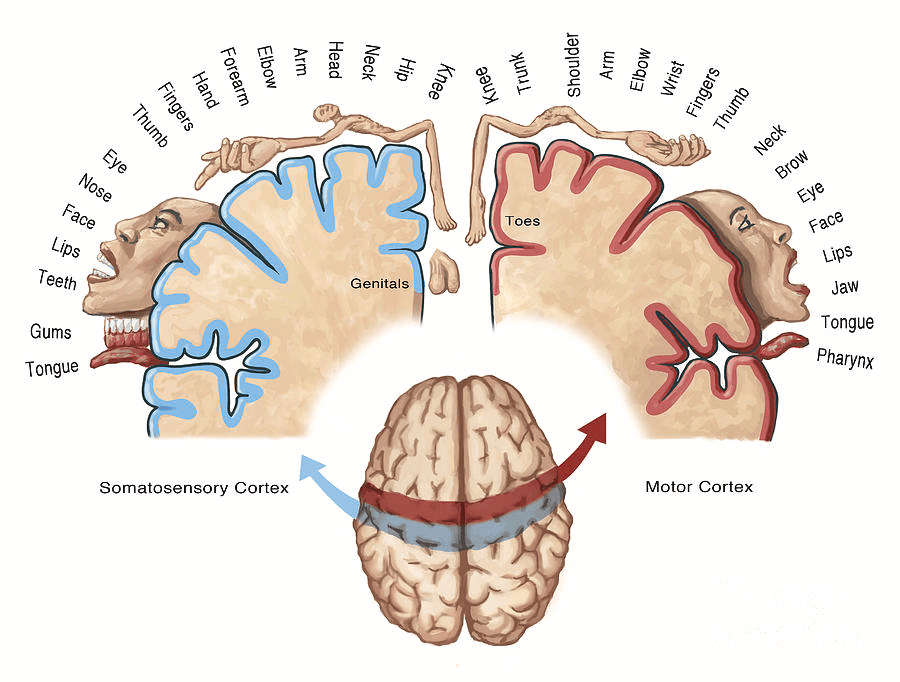
I am not sure if this image is free use, it came from a website for print purchase, perhaps our brainbook team could draw something similar?
The last type of central neural mechanism is the body schema concept. This is the idea that a template of the entire body can be found in the brain, and any changes to the body that cause a mismatch between it and the template results in perception of a phantom limb. Neurosignature is similar to this, where intentional actions such as moving the amputated limb cannot be executed and lead to stimulation in the parietal and frontal lobes to cause pain.
Key Clinical Features
Onset of pain in the amputated limb can occur immediately or years after the amputation. Features include:
- Throbbing
- Piercing
- Pins and needles
- Tingling
Risk Factors
A number of factors cause someone to be more likely to experience phantom limb pain. These include:
- If the amputation is at an upper extremity
- Presence of preamputation pain
- If the limb comes in a pair, residual pain in the remaining limb not amputated
- Time closely following the amputation
- Female sex
As we can see, not many of these are able to be controlled.
Treatment
Treatment seeks to minimise pain and rehabilitate the patient. The best approach is multidisciplinary.
- Medications include opioids, tricyclic antidepressants, anticonvulsants, sodium channel blockers and NMDA receptor antagonists
- Surgical management includes revision surgery, nerve block and central nervous system stimulation
- Alternative treatment includes mirror therapy, massage, cognitive behavioural therapy for pain management and prosthesis training
Prognosis
Prognosis varies greatly between patients, from a few months to decades. Engagement in and enthusiasm for the treatment options helps to speed up the rate at which the symptoms diminish.
Key Takeaway Messages
- Phantom limb pain is pain following amputation of a body part
- There are 3 main theories for phantom limb pain: a psychogenic mechanism, a peripheral mechanism and a central neural mechanism
- The central neural mechanism is the most commonly accepted theory, where the spinal cord or brain adapts to accommodate the amputation, but this leads to a mismatch in the brain’s template of the body, which causes pain when actions cannot be carried out or sensation is passed onto the amputated limb and cannot be contextualised
- Key clinical features of phantom limb pain are varying sensations in the amputated limb, from tingling to throbbing sensations
- The risk factors are not generally modifiable
- Treatment is multidisciplinary, with medications, surgery and therapies all showing effect based on the patient and their engagement in the treatment
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3198614/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6003018/
https://pubmed.ncbi.nlm.nih.gov/16012411/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6354174/
Credits
Fatima
Brainbook Editorial Officer

Leave a Reply