Introduction
A limp. Blurry Vision. Poor speech. Uncontrollable laughter. Altered personality. Excessive thirst and hunger. Lethargy. Vomiting. Headache. Weakness. Seizures….
Anything that the brain controls, brain tumours can impact.
Brain tumours are the leading cause of paediatric cancer-related morbidity and mortality and the 2nd most common cause of paediatric cancer following leukaemia. Most paediatric brain tumours are primary, meaning they originate within the central nervous system (CNS).
Symptoms of Paediatric Brain Tumours By Location
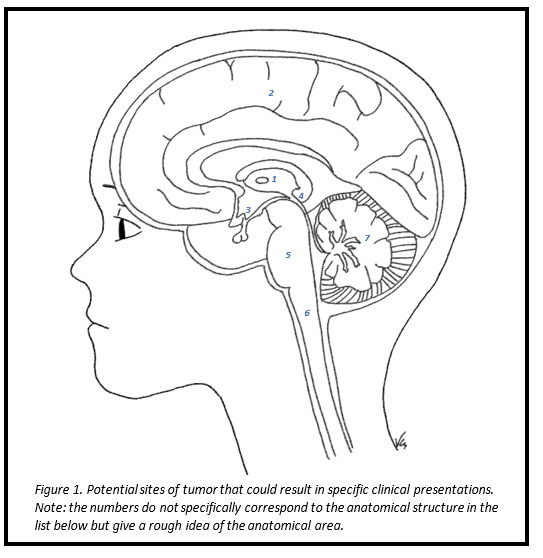
Supratentorial
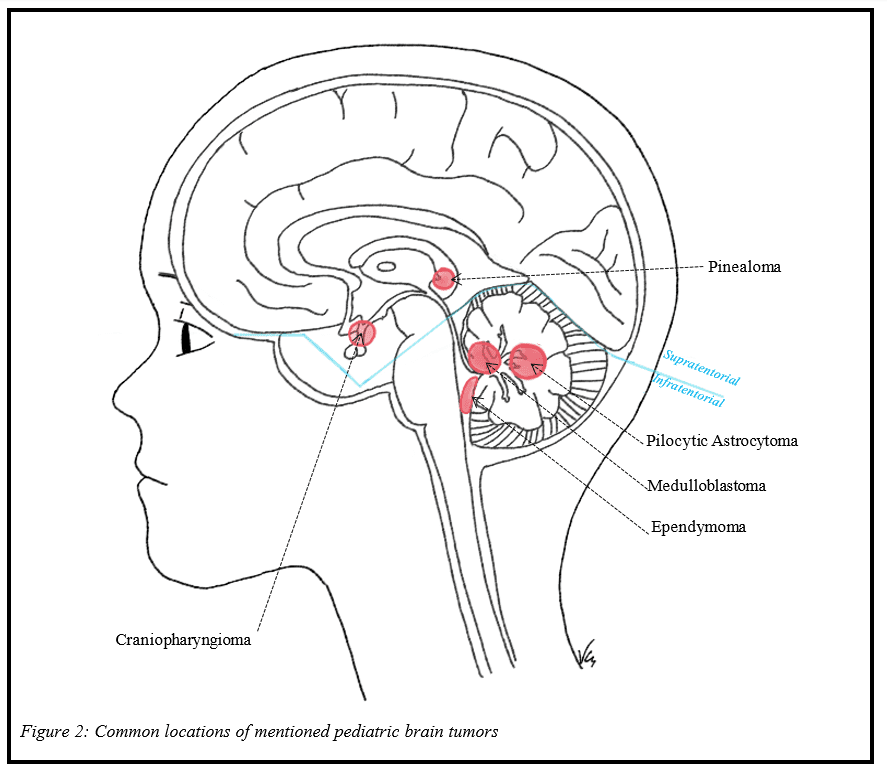
(Supratentorium refers to the upper part of the brain relative to an extension of the dura mater – part of the linings of the brain – known as the tentorium cerebelli. This acts as a roof separating the cerebellum from the inferior parts of the occipital lobe of the brain. The separation between supratentorium and infratentorium is visualised in Figure 2., by the blue line)
- Thalamus/Basal Ganglia
- Hydrocephalus
- Movement disorders
- Numbness, weakness, tingling on the opposite side of the lesion
- Cortex
- Seizures
- Altered personality.
- Aphasia (impairment of language)
- Motor disorders
- Intellectual impairment
- Visual deficits
- Memory Impairment
- Hallucinations
- Encephalopathy
- Suprasellar Region (includes the pituitary gland)
- Visual Field deficit (Bitemporal hemianopsia – vision is missing in the outer half of the right and left visual field)
- Compression of hypothalamic pathways: Delayed Puberty, Anorexia, Eating disorders, Diabetes Insipidus (characterised by increased thirst and large amounts of urine), Short stature
- Pineal/Midbrain Tectum
- Vertical gaze palsy (inability to move their eyes up and down)
- Hydrocephalus
- Vomiting
- Double Vision
Infratentorial
Infratentorial refers to the lower part of the brain and consists of the cerebellum. This is visualised in Figure 2.
- Pons:
- Double Vision
- Weakness
- Incoordination
- Inability of eyes to move in the same direction
- Facial Weakness
- Drooling
- Cervicomedullary Junction:
- Horner Syndrome – combination of features due to the disturbance of a group of nerves: constriction of the pupil, upper eyelid droop, absence of sweating and posterior displacement of the eye)
- Weakness
- Swallowing problems
- Abnormal voice
- Tilting of the head
- Cerebellum
- Ataxia (Slurred and/or scanning speech, incoordination, falling)
- Vomiting
- Dysmetria (lack of coordination and accuracy in voluntary movements)
- Repetitive, involuntary rapid movements of the eyes. Often called “dancing eyes” (Nystagmus)
- Tremor
Tumour Types
Please note, this is not an exhaustive list of the types of pediatric tumours.

Posterior Fossa/ Infratentorial Masses: (60%)
Pilocytic Astrocytoma
Pilocytic astrocytomas (PAs) are the most common benign pediatric brain tumours.
- Age: Children and young adults (<20 yrs)
- Typical Location: Posterior cranial fossa (infratentorial)
- Classic site for PAs is in the cerebellum, but can present anywhere in CNS such as the cerebral hemispheres or hypothalamus
- Associations: Neurofibromatosis type 1 (NF1) [for more information on neurofibromatosis, refer to Brainbook link]
- Prognosis:
- Excellent with an overall survival time of 20 years
- Can be wholly curable with complete surgical resection.
- Recurrence common if lesion is in hypothalamus due to excision difficulty.
Medulloblastoma
Medulloblastomas are invasive, highly malignant embryonal tumours of the posterior fossa and the most common malignant pediatric brain tumour (20 – 25% of all cases).
- Age: <20 years with peak incidence between 5 to 8 years (1st decade)
- Typical Location: Cerebellum (infratentorial) and fills the 4th ventricle (one of the interconnected fluid filled cavities in the brain)
- Prognosis:
- High risk patients include patients less than 3 years of age, large residual tumour after surgical resection, and occurrence of drop metastasis (metastasis down the spinal cord).
- 60 – 80% 5-year survival rate
Ependymoma
Ependyomas arise from cells that link the ventricular system, are the 3rd most common brain tumours in children contributing to 30% of intracranial tumours in children under 3 years.
- Age: peak age of occurrence is in the first decade
- Typical location: 90% of ependymomas in children are intracranial and most commonly appears in the 4th ventricle with 2/3rds of the tumour in the posterior fossa. The next common sites include supratentorial locations involving lateral ventricles (paired cerebrospinal fluid filled spaces in the cerebellum and part of the ventricular system).
- Associations: Neurofibromatosis Type 2 (NF2). [for more information on neurofibromatosis, refer to Brainbook link]
- Prognosis:
- Usually poor prognosis with 60-95% overall 5-year survival rate.
Supratentorial tumors (40%)
Craniopharyngioma
Craniopharyngioma are rare, slow growing benign epithelial tumours that originate from embryonic remnants of the Rathke pouch in the suprasellar region (supratentorial). (Rathke’s pouch refers to the place where the anterior and posterior pituitary gland meet. This usually closes in fetal development but remnants can persist.)
- Age: peak at 5 to 14 years and at 50 – 75 years
- Typical Location: Supratentorial; in the 3rd ventricle (one of the cavities that is part of the ventricular system)
- Prognosis:
- Typically good, with a 90% 10 year survival rate
- Recurrence rate is high.
Pinealoma
Tumours arising from cells in the pineal gland are known as pinealomas, and comprise less than 2% of all childhood brain tumors.
- Age: typically, in younger children (<5 yrs)
- Typical location: The pineal gland is located in the posterior 3rd ventricle and pineal tumours often present with non-communicating hydrocephalus due to compression of the cerebral aqueduct. [for more information on hydrocephalus, refer to this article on Brainbook]
- Prognosis: Pineocytomas – the most benign of all pineal parenchymal tumours has a 86% 5 year survival rate.
Investigations
Children presenting with signs and symptoms indicative of intracranial disease require a thorough examination by a specialist. Primary investigations include full history, physical examination, and neuroimaging studies.
Neuroimaging: Altered mental status, cognitive decline or behavioural changes in association with headache, nausea, vomiting and ataxia in the absence of infection should be referred to an urgent CT scan.
- CT with contrast is the most common screening tool of the brain and spine
- MRI with contrast:
- Test of choice and is the most sensitive neuroimaging modality for detecting a brain tumour
- Preferred choice for subsequent follow up in children receiving treatment
Blood Tests: Primary Brain Tumours typically do not produce blood abnormalities as opposed to CNS metastases which may present with systemic features of malignancy.
Other investigations:
- Endocrine laboratory tests
- Ophthalmologic exam: Papilledema (optic nerve swelling) is the most reliable sign of increased ICP (increased intracranial pressure). This is common with tumours that causes occlusion to CSF flow.
- Urine Tests
Management
Management requires a multidisciplinary approach including neurosurgeons, oncologists, social workers, pediatric psychiatrists, radiologists, nurses, to name a few. The strategy of treating pediatric brain tumours is typically a combination of surgery, chemotherapy and radiation. Other considerations include: steroids, seizure prophylaxis, and workup for any concurrent illnesses.
Surgery
Surgery remains the first approach for most pediatric brain tumours, enabling histological analysis, intracranial pressure relief and resection of tumors. In most cases, near-total resection can be accomplished. Preoperative MRI or CT imaging, intraoperative MRI imaging and neurophysiologic monitoring of visual, auditory and sensory pathways help minimise manipulation of normal brain tissue during surgical resection. Postoperative imaging by MRI is done within the first 24 to 72 hours to ensure there are no complications and to plan for adjuvant therapy.
Chemotherapy
Chemotherapy is given as the primary postoperative therapy for most tumours but is also used as the primary treatment for young children with tumours in their hypothalamus and in the optic pathway.
Radiation
- 3 years of age: adjuvant to chemotherapy and surgical resection
- <3 years: Due to the risk of severe damage to the developing brain, radiation is usually avoided in children younger than 3 years.
Pallative Care
- In cases of poor prognosis it is important to involve palliative care early on to provide support, guidance and comfort measures for the child and their loved ones and for action to be taken so that the child’s goals and wishes are achieved.
Brainbook Resources:
- For more information regarding hydrocephalus and shunts please visit: Hydrocephalus, VP Shunts
- For more information on brain tumors please visit: (Brainbook link)
References:
- Naga O. Pediatric Board Study Guide. Cham: Springer International Publishing; 2020.
- Adesina A, Tihan T, Fuller C, Poussaint T. Atlas of Pediatric Brain Tumors. Cham: Springer International Publishing; 2016.
- Udaka YT, Packer RJ. Pediatric brain tumors. Neurologic clinics. 2018 Aug 1;36(3):533-56.
- Wells EM, Packer RJ. Pediatric brain tumors. CONTINUUM: Lifelong Learning in Neurology. 2015 Apr 1;21(2):373-96.
Credits

Vanessa Chow
Brainbook Editorial Officer
At the time of writing, Vanessa is a final-year medical student at St George’s University of London.

Leave a Reply