What is Meningitis?
Meningitis is an inflammatory process involving the meninges and is one of the most common infectious disease emergencies involving the central nervous system (1)
The meninges refer to the coverings of the brain and spinal cord. There are three layers and from the layer closest to your skull, these are termed: dural mater, arachnoid mater and pia mater. The dura mater is also known as the pachymeninges, the arachnoid and pia combined are referred to as the leptomeninges and the space between the arachnoid and pia mater is called the subarachnoid space.
Retrieved from https://www.thoughtco.com/brain-anatomy-meninges-4018883 03.08.2022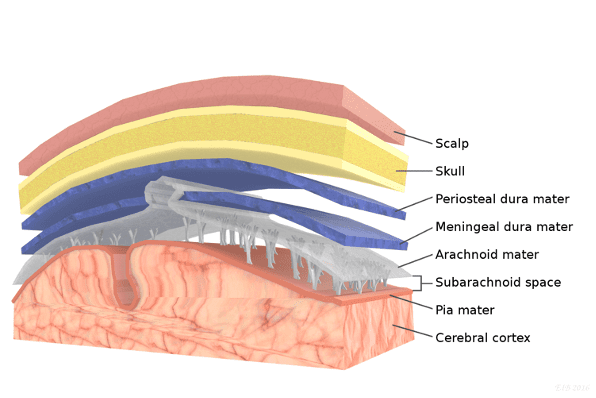
In infectious meningitis, the leptomeninges are typically affected but pachymeningeal involvement can be seen in fungal, tubercular, and syphilitic meningitis. The introduction of pathogens into the subarachnoid space activates the immune system causing the clinical features seen in meningitis.
Meningitis can occur in non-infectious contexts such as chemical meningitis in which inflammation can occur as a response to irritants such as debris from a ruptured cyst, or carcinomatous meningitis, because of metastatic cancer cells reaching the subarachnoid space (2)
In this article, infectious, particularly bacterial meningitis will be discussed.
So, who is at risk for meningitis?
Monitoring and detecting people at risk of infectious disease, especially to the central nervous system is crucial for early diagnosis, management and thus a favourable outcome. In the context of meningitis, risk factors include:
- People in an immunocompromised state (elderly patients, HIV patients, cancer patients, transplant recipients, diabetic patients)
- CSF leak after cranial injury or a surgical intervention
- Site-specific infections such as pneumonia, sinusitis, otitis media
- Septic patients
- Maternal Group B streptococcal infection during birth
- People living in crowded conditions
- Close contact with an infected individual
Pathophysiology (1, 2)
People at a higher risk of meningitis, are in other words, more susceptible to pathogen entry, and in most cases, the causative pathogen colonises the nasopharynx or the upper airways before entering the CNS, or via direct infection due to trauma or head surgery.
Common microbes
The most common organisms that cause bacterial meningitis vary with the patient’s age.
- In neonates, common causative agents include: E.coli, and Group B streptococci.
- In adolescents and young adults, Neisseria meningitis is the most common organisms
- In older adults, Streptococcus pneumonia and Listeria monocytogenes are more common
- Immunocompromised patients are at particular risk for Listeria monocytogenes meningitis.
Common causative agents for viral meningitis include:
- Enteroviruses, which is one of the leading causes of viral meningitis, and infants and young children are common victims of enteroviral meningitis (1)
- Other common viruses include: Herpes Viruses Measles, Influenza, HIV(1)
Signs and Symptoms
Duration of symptoms may be acute (< 5 days), subacute (6 – 30 days), or chronic (>30 days) with clinical manifestations dependent on the age of the patient, their medical history as well as the virulence of the causative organism and the site of infection.
The classic features include:
- Fever
- Headache
- Meningismus which a clinical triad of headache, neck stiffness and photophobia
- An altered mental status that ranges from lethargy to stupor, obtundation or coma. The change in mental status secondary to meningitis is referred to as meningoencephalitis
- Nausea and vomiting
All four of these features, according to a study are only present in 45% of patients, while 95% of patients will have at least two of the four. (van de Beek et al., (2004)) Elderly patients may present in the absence of fever or meningeal signs.
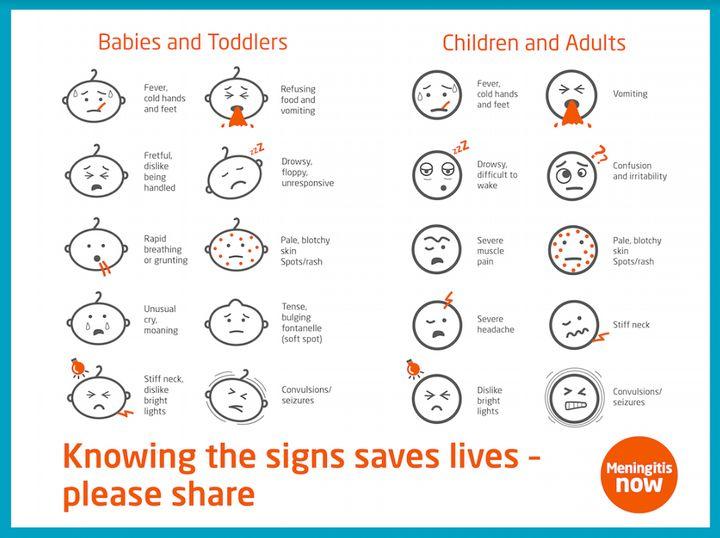
Retrieved from: https://www.huffingtonpost.co.uk/entry/meningitis-babies-children-symptoms-treatment_uk_57dbff58e4b05d79136f9590 09.08.2022
In addition, neonates may present with:
- Lethargy, irritability, and excessive crying
- Gastrointestinal symptoms like vomiting, diarrhoea, and poor feeding
- Respiratory distress and apnoea
- Seizures
- Bulging fontanelle
- A non-blanching rash should raise suspicion of meningococcal meningitis
- Signs of meningeal irritation are collectively referred to as meningismus and these include certain signs:
- Nuchal rigidity (stiffness of the neck)
- Kernig sign – pain on passive knee extension with the hip flexed
- Brudzinski sign – hip and knee flexion with passive neck flexion
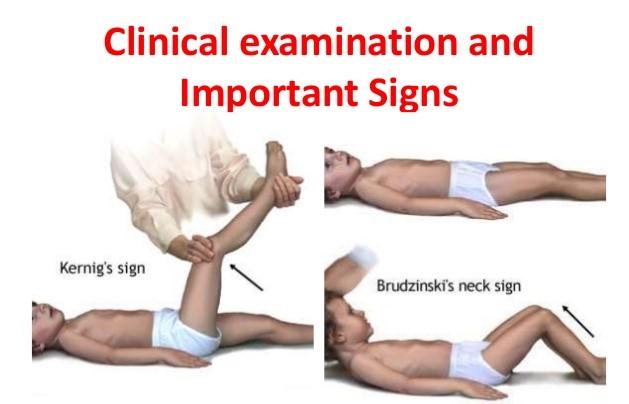
Retrieved from: https://blog.ucbmsh.org/department/clinical-examination-important-signs-of-meningitis 09.08.2022
These signs may be absent in patients over the age of 65 years, in immunocompromised individuals or in those taking analgesic medications.
In patients suffering from viral meningitis, their mental status is usually intact, and the duration of symptoms is relatively longer compared to bacterial meningitis.
Initial Management (1–3)
Bacterial meningitis is a neurologic emergency and universally fatal if left untreated. Outcomes and complications are worse with delayed treatment! Odds of an unfavourable outcome may increase by 30% for each hour of treatment delay Therefore, diagnostics and treatment need to be initiated simultaneously.
The suspicion of meningitis should, without delay, prompt:
- Initiation of empirical antimicrobial and dexamethasone therapy
- Treating shock, airway, and seizures if the patient is hemodynamically unstable
- Establishment of IV access, administration of oxygen if necessary and screening for organ dysfunction
- Bloods for: Culture, glucose, WBC, and coagulation studies
- Confirmation of CSF analysis is done by cerebrospinal fluid (CSF) examination via a lumbar puncture and is essential for precise microbiological diagnosis and antibiotic susceptibility testing. Once this information is available targeted antimicrobial therapy can be switched from empirical. However, if there are signs of elevated intracranial pressure, a lumbar puncture may be unsafe to do.
- In such cases, neuroimaging such as Computed Tomography (CT) is done before the lumbar puncture to rule out increased intracranial pressure. Assessing if LP should be done or not requires clinical judgement and imaging can help reach the decision.
The mainstay treatment for bacterial meningitis is antibiotics. Due to the delay in this process, empirical antimicrobial treatment should be initiated immediately. The antibiotic regimen is then adjusted according to the known causative organism identified on blood and CSF cultures.
In viral meningitis, management is supportive. For those with suspected Herpes Simplex Virus (HSV) infection, empiric antiviral therapy is initiated to prevent complications of HSV encephalitis.
Management of bacterial meningitis typically requires hospitalisation for at least a week. Viral meningitis is usually self-limiting, resolving in 7 – 10 days and often can be treated at home.
CSF findings – reaching the diagnosis
Patterns of abnormalities in the cerebrospinal fluid can aid in distinguishing the causes of meningitis.
Three major factors of CSF help physicians and microbiologists paint the picture of the cause:
- CSF glucose:
- Low CSF glucose (hypoglycorrhachia) alerts physicians to an infectious aetiology, most commonly bacterial, tuberculosis and fungal meningitis. CSF glucose is typically normal in viral meningitis, but low CSF glucose levels may be seen in some viruses (mumps, lymphocytic choriomeningitis virus, West Nile virus, enterovirus, and cytomegalovirus (CMV) in association with HIV/AIDS.) Low CSF glucose can also be present in the neoplastic process, inflammatory conditions such as sarcoidosis, chemical meningitis, and subarachnoid haemorrhage.
- CSF protein:
- CSF protein is typically elevated in meningitis and the degree of CSF protein elevation is reflective of the extent of opening of the blood-brain barrier caused by bacterial infiltration.
- Cell type Predominance:
- The types and degree to which these cells are found in the CSF allude to the type of infection.
This diagram provides a useful summary of the differences in the CSF fluid that help determine the cause of meningitis: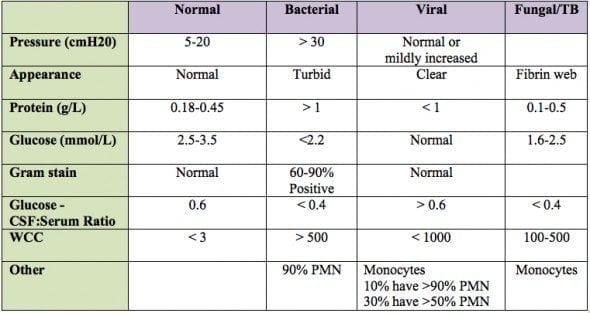
Retrieved from: https://litfl.com/csf-analysis/ 09.08.2022
So, what can you do to prevent you or those around you from getting meningitis?
Vaccination (6)
Meningitis can be caused by different infections and so there are several vaccinations that are available for its prevention. The list below outlines the offered vaccines in accordance with the UK NHS system.
- Meningitis B vaccine
The meningitis B vaccine offers protection against meningococcal group B bacteria which as listed above is a common cause of meningitis in young children in the UK
The vaccine is recommended for neonates aged 8 weeks, followed by the second dose at 16 weeks and a booster at 1 year.
- 6 in 1 vaccine
This vaccine is also referred to as the DTAP/IPV/HiB/Hep B vaccine and protects against diphtheria, tetanus, whooping cough, hepatitis B, polio, and Haemophilus influenza type b (Hib).
It is offered three times at 8, 12, and 16 weeks.
- Pneumococcal vaccine
This vaccine protects against infections caused by pneumococcal bacteria and is offered at 12 weeks with a booster at 1 year of age.
- Hib/MenC vaccine
This vaccine protects against meningococcal group C bacteria which can cause meningitis and is offered as a combined vaccine at 1 years old.
- Meningitis ACWY
Teenagers and students going to university for the first time are advised to have the meningitis ACWY vaccine, which protects against meningococcal groups A, C, W and Y.
- MMR vaccine
This vaccine protects against measles, mumps and rubella which can result in meningitis. It is offered at 1 years of age, with a second dose at 3 years and 4 months.
What if someone I am in close contact with has meningitis?
In that case, antibiotics for prevention are typically offered. The antibiotics given differ depending on the bacteria causing the infection.
Meningococcus
- Antibiotics promptly decrease the risk of transmission for close contacts of those with meningococcal disease. This is usually recommended for close contacts within the household where ciprofloxacin is the antibiotic of choice
Group B Streptococcus
- Identification of mothers whose babies are at risk of getting Group B streptococcus can be done by universal screening for carriage of Group B streptococcus in pregnancy. Mothers at risk are often offered IV penicillin during labour to prevent their babies from developing Group B streptococcal infection.
Complications
The most common complication of meningitis is hearing loss. This may be transient or permanent.
Other complications may include:
- seizures,
- cognitive deficits
- cerebral oedema,
- cerebrovascular disease,
- brain abscess,
- increased intracranial pressure.
The prognosis (2)
Poor prognosis is associated with coma, seizures, hypotension, pneumococcal aetiology, respiratory distress, delay in treatment and certain CSF findings including:
- A CSF glucose level of <0.6mmol/L (<10mg/dL)
- A CSF protein level of >2.5 g/L
- WBCC of <5000/uL
Moderate or severe complications occur in ~25% of survivors and include decreased intellectual function, memory impairment, seizures, hearing loss, dizziness and gait disturbances.
Remember to:
Get medical advice as soon as possible if you are concerned you or your child could have meningitis. Remember the symptoms of meningitis can mimic ones of the flu, especially in elderly people.
References:
- Hasbun R, editor. Meningitis and Encephalitis. Cham: Springer International Publishing; 2018.
- ’Kumar V “Abbas, AK” “Aster, JC.” Robbin’s Basic Pathology. 10th ed. Philadelphia, PA: Elsevier – Health Sciences Division; 2017. 862–864.
- Aksamit AJ, Berkowitz AL. Meningitis. CONTINUUM: Lifelong Learning in Neurology. 2021 Aug;27(4).
- Wissman K, Ferdock A, Skef S, Shelesky G. Does dexamethasone improve outcomes in adults with bacterial meningitis? Evidence-Based Practice. 2020 Aug;23(8).
- Jameson J, Kasper D, Longo D, Fauci A, Hauser S, Loscalzo J. Harrison’s principles of internal medicine. 2018.
- Meningitis – Vaccination [Internet]. nhs.uk. 2021 [cited 13 November 2021]. Available from: https://www.nhs.uk/conditions/meningitis/vaccination/

Leave a Reply