An awake craniotomy (AC) is a surgical procedure to remove part of the bone from the skull and expose the underlying brain, while the patient is awake for a certain duration of the procedure.
Awake craniotomies have been tied to beneficial outcomes as compared to a craniotomy whereby the patient is under general anaesthesia for the full duration of the procedure. These beneficial outcomes are:
- Greater extent of tumor resection
- Fewer neurological deficits
- Shorter hospital stay and longer survival
AC was initially used as a surgical intervention for epilepsy. Surgeons used it to localize the origin of epileptic activity in the brain. This was a form of mapping of the brain cortex. Today, ACs are used for:
- Resection of tumors which could be near the areas of the brain associated with motor and language functions
- Ventriculostomy (a neurosurgical procedure whereby a hole is made in a ventricle—one of the fluid-filled cavities of the brain—to facilitate drainage).
- Stereotactic brain biopsies (a surgical procedure where a thin needle is inserted into the brain by a neurosurgeon to extract a small piece of tissue to examine under a microscope.)
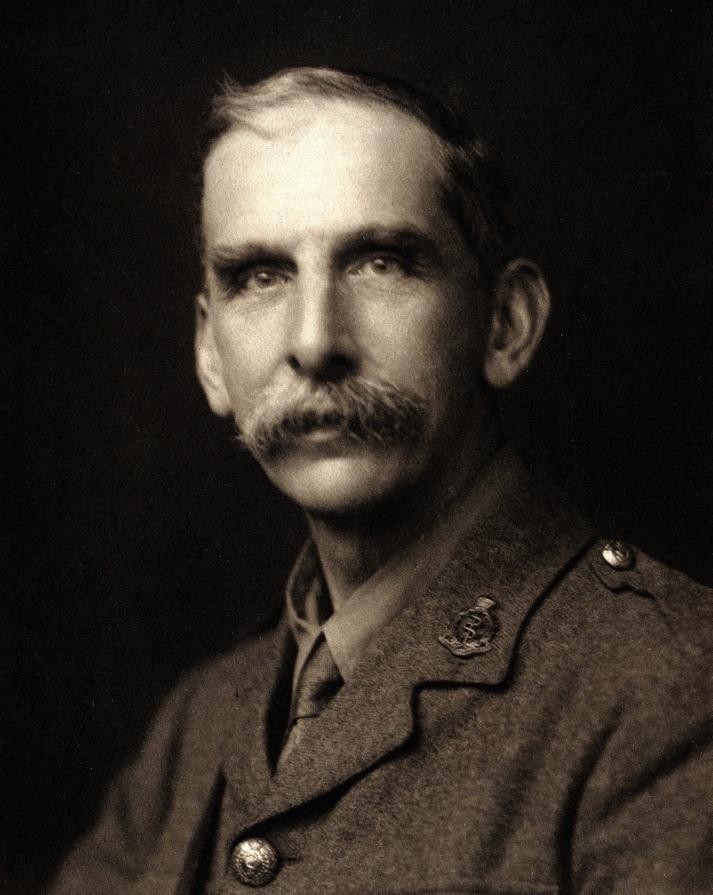
The first known recorded AC was done in 1886 by Sir Victor Alexander Haden Horsley, to treat a patient with epilepsy who went on to make a significant recovery. Horsley famously said, “I have not employed ether in operations on man fearing that it would tend to cause cerebral excitement; chloroform, of course, producing, on the contrary, well marked cerebral depression.”
Sir Victor Alexander Haden Horsley (1857- 1916). https://en.m.wikipedia.org/wiki/Victor_Horsley
Wilder Penfield of Canada made mappings in conscious patients with severe epilepsy under local anaesthesia (LA) at the Montreal Neurological Institute by directly assessing brain response to electrical stimuli.
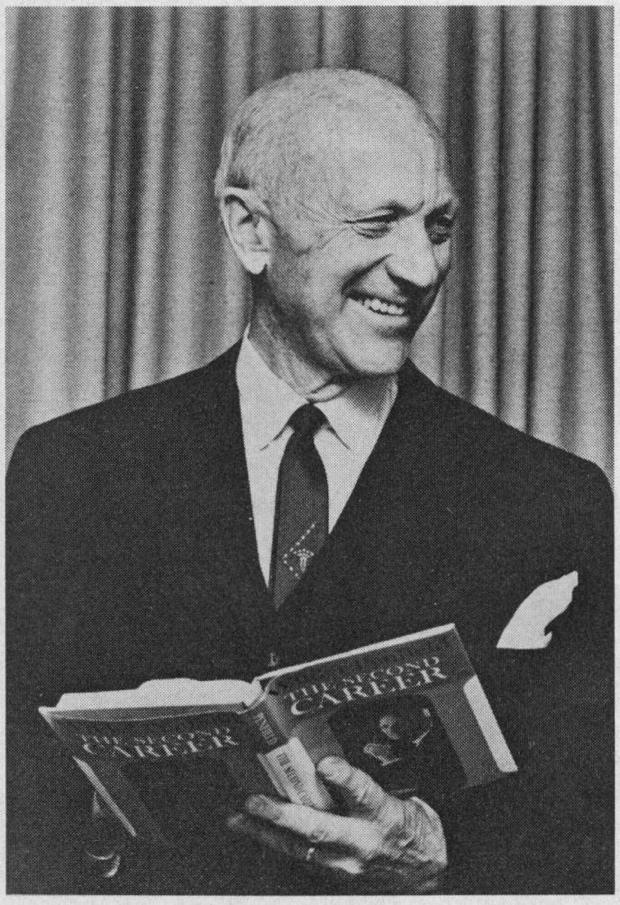
Wilder Graves Penfield (1891-1976) https://www.researchgate.net/figure/Wilder-Penfield-at-the-publication-of-his-hook-of-essays-entitled-The-Second-Career_fig3_22812351/amp
As early as 1928, Otfrid Foerster in Germany was using ether anaesthesia and electrical stimulation of cortex to reproduce patients’ seizure activity.
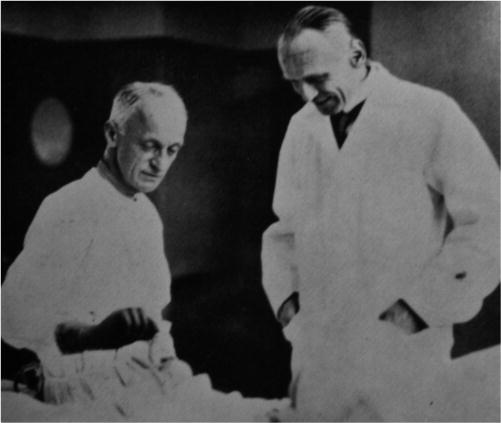
Harvey Cushing and Otfried Foerster https://thejns.org/view/journals/j-neurosurg/107/2/article-p451.xml
In 1929, German psychiatrist Hans Berger published his landmark paper on the EEG(Electroencephalogram, a machine used to show brain wave activity). This and similar research by Herbert Henri Jasper and Frederic Andrew Gibbs showed how such a device could be used to accurately localize the focus of epileptic activity in the brain. This strengthened the argument for AC.
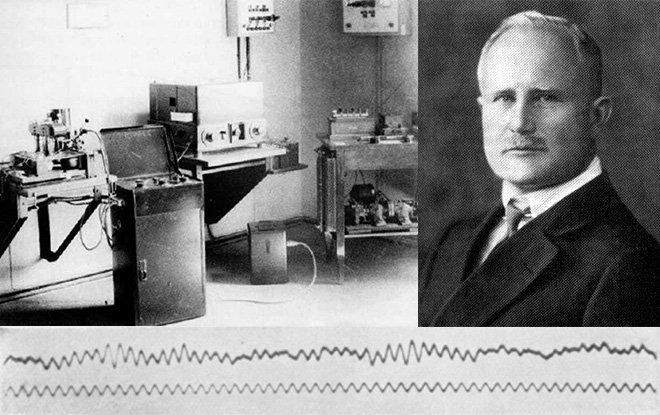
Hans Berger (1873-1941)
Wilder Penfield and Herbert Henri Jasper (standing)
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1528-1167.2009.02043.x
Frederic Andrew Gibbs (1903-1992)
A very strong argument for AC is that the neurosurgeon can operate and do cortical mapping at the same time, hence greater extent of tumor resection and lower risk of neurological damage due to surgery.
What exactly is cortical mapping?
Cortical mapping is simply a procedure by which electrical stimulation using electrical probes is applied to the surface of the brain so as to identify which areas of the brain are important for motor function (movement of various body parts), sensory function (how you perceive sensation) and language function.
Mapping is done by the neurosurgeon stimulating the relevant cortical areas with electrical probes and then evaluating the patient’s response.
Providing anaesthesia for AC requires:
- Pain relief to the scalp (to cover the initial incision made)
- Sedation for the patient
- Airway management
Patient selection
The patient selection for an AC should be coordinated between the neurosurgeon and the anaesthetist. The patient should be evaluated in the pre-operative assessment clinic to establish whether they can psychologically manage the procedure awake, and whether there are any medical conditions that would make it excessively risky.
The reason for this careful selection is that abandoning the awake operation and putting the patient to sleep in the middle of operation could lead to complications and is extremely distressing for the patient.
If the patient is unwilling to undergo the procedure or is claustrophobic, then the procedure should be done asleep.
Relative contraindications to awake craniotomy are:
- Anxiety disorders
- Dysphagia (difficulty swallowing)
- Confusion or somnolence
- Alcohol or drug dependency
- Chronic pain disorders
- Restless leg syndrome
- Low pain tolerance
- Morbid obesity
- Obstructive sleep apnoea (a condition whereby one is suddenly unable to breathe during sleep. Can lead to death).
- Uncontrolled cough
- Tumors of blood vessels or umors close to major crucial blood vessels, whose resection could lead to high blood loss.
Routine antiepileptic drugs for seizure prevention and management are not given as they can affect test by causing sedation. In some centres, patients are allowed to use anti-epileptic drugs preoperatively (before the operation) until the day of the operation.
Preoperative preparation of the patient
Patients at risk of development of airway obstruction (morbid obesity, obstructive sleep apnoea) due to sedation are identified preoperatively and evaluated for elective or emergency airway management.
Psychological preparation of the patient, by explaining the procedure to them, is crucial to ensure patient cooperation during AC. The full operative team meets the patient and explains the procedure to them and build rapport. As for premedication, if the indication for AC is epilepsy, antiepileptics are usually withheld to facilitate cortical mapping. Drugs to alleviate anxiety are also given, but this should not be a substitute for psychological preparation of the patient.
Intraoperative care of the patient
Patient monitoring is critical during AC, so the patient will have numerous machines and monitors attached to them. The patient is positioned on the operating table, and if the scalp block (local anaesthetic injection to the scalp) is to be used it is delivered then, either by the anaesthetist or the surgeon.
Once the patient is numb, the Mayfield clamp (see figure B) can be be applied painlessly to immobilise the patient’s head and neck, and the patients scalp will be shaved, sterilised (washing andapplication of a solution to kill any bacteria present on scalp to prevent infection) and draped. This whole process may be done with the patient fully anaesthetised, lightly sedated or fully awake.
The advantage of a pinned head frame is that it prevents the head from moving. The disadvantage is that it makes the manipulation of the head and neck in case of an airway emergency difficult.
The patient at this point is usually on their back or turned slightly to the side.
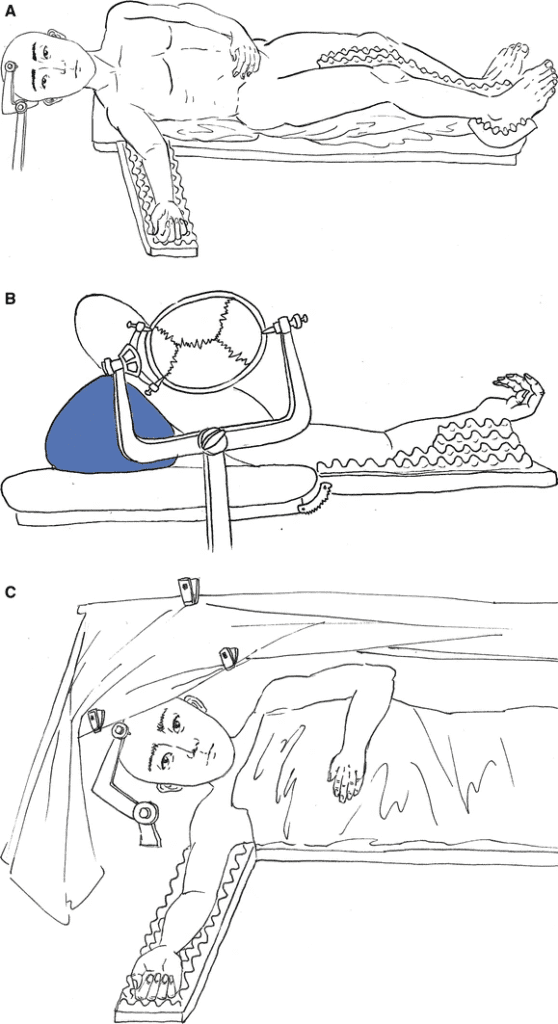
https://link.springer.com/article/10.1007/s12630-017-0840-1
Techniques of anaesthesia for awake craniotomy
The patient can be fully awake throughout the whole procedure (AWAKE-AWAKE-AWAKE)
The other technique involves general anaesthesia being used at the beginning and end of the operation (ASLEEP-AWAKE-ASLEEP) or only at the beginning (ASLEEP-AWAKE).
- AWAKE-AWAKE-AWAKE
Moderate sedation is given for the painful parts of the procedure (application of Mayfield Pins, skin incision, removal of the bone flap during the actual craniotomy, opening of the dura which is the outer covering of the brain). Sedation will then be reduced or stopped during cortical mapping and will be restarted during cortical closure. The sedation makes the procedure tolerable, especially during the awake phase when cortical mapping is being done.
- ASLEEP-AWAKE-ASLEEP
General anaesthesia (whereby the patient is sedated to unconsciousness for the purpose of the operation) is done at the start of the operation and the airway secured with a device called an endotracheal tube to enable the patient to breathe during the operation.
Once the previously mentioned painful parts of the operation are done, the patient is awakened for the purpose of cortical mapping. General anaesthesia is then induced again once cortical mapping is done.
If the patient’s airway is secured with the endotracheal tube, sometimes the patient could cough or be agitated during the awake phase. This could lead to brain swelling and interference with surgery.
For this reason, another airway device called a Laryngeal Mask Airway (LMA) is used. It enables smoother transition from one phase to another.
A few final considerations
For the post-awake phase, lower rates of sedative infusion are needed. This could be due to:
- Fatigue from the procedure means the patient goes under easily.
- Relief of patient from psychological pressure after learning of successful resection of the brain lesion
- Lower level of painful stimuli during skull closure than in skull opening.
Awake phase (considerations)
Once sedation or GA have been used in the pre-awake phase, preparations to wake the patient should begin. The surgeon will usually have given a time estimate for waking the patient.
All sedative and hypnotic agents are usually discontinued as soon as the bone flap is removed. The goal is to wake the patient smoothly without confusion, agitation or drowsiness.
Some anaesthesiologists use an anaesthetic agent called remifentanil at low rates of infusion to ensure smooth transition into wakefulness.
If the pre-awake phase was done under GA or deep sedation, agitation on waking, which is potentially dangerous, can occur. If it does, re-induce anaesthesia is re-induced with an anaesthetic agent called propofol. Another anaesthetic agent called dexmetomidine is used prior to the second wake-up attempt. A low rate remifentanil infusion can be used on reawakening to help with behavioural control. Somnolence (excessive drowsiness) on emergence can also occur. Intravenous (through the vein) caffeine can be given. We all know what a good pick-me-up caffeine is!
For the awake phase, there are some key points:
- Keep the patient engaged and cooperative
- Wet the patient’s lips with ice-cold water, or give them ice chips to suck on.
- Scratch the skin around the patient’s nostrils and corners of the eye. This is because opioid-related itching is a common occurrence.
- Use an air blanket for the patient to either keep them warm or cool them down.
- Adjust room temperature to the patient’s liking and comfort.
- Empathy, hand-holding and reassurance.
- Bilingual patients may need bilingual language testing as part of language mapping.
Intraoperative complications
Seizures. Fortunately, many of these are brief, involve a specific body part(s) and resolve spontaneously. Some, however, may involve the whole body.
Post awake phase
Sedation is restored and the AC can usually be finished without an LMA, even if it was used in the pre-awake phase. As stated, lower rates of sedation are usually needed in the post-awake phase.
Postoperative care
AC usually has a shorter hospital stay of about 4 days, as compared to craniotomy under general anaesthesia (about 9 days). There have actually been reports of patients who have undergone AC being discharged on the same day as when surgery was done! Amazing, right? After the procedure, the patient can be admitted to the neurointensive care unit (neuro-ICU) for close overnight observation. In some quarters, however, this is considered overly conservative.
REFERENCES:
https://link.springer.com/article/10.1007/s12630-017-0840-1
https://www.ncbi.nlm.nih.gov/books/NBK572053/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7713838/
https://en.m.wikipedia.org/wiki/Victor_Horsley
https://thejns.org/view/journals/j-neurosurg/107/2/article-p451.xml
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1528-1167.2009.02043.x

Leave a Reply